With eyes shut tight and minds drifting into the realm of deep slumber, we embark on a nocturnal journey filled with vivid thoughts and mental landscapes. These subconscious expeditions, often known as dreams, hold a multitude of mysteries waiting to be unraveled. However, have you ever considered the impact that head injuries can have on this ethereal realm of sleep?
When the brain, the epicenter of our thoughts and emotions, sustains a blow, it is not just the physical repercussions that need attention. The intricate network of neurons that governs our sleep cycles and dreaming patterns can be profoundly affected. This intricate relationship between head injuries and sleep presents a compelling avenue of exploration, delving into how these traumas disrupt the delicate balance between wakefulness and rest.
Traumatic head injuries, be it a bump, blow, or jolt to the head, can thrust individuals into a world where their thoughts remain persistently scattered, and peaceful sleep becomes an elusive entity. Such injuries often result in a tumultuous cascade of changes within the brain, impacting the neurotransmitters and hormones responsible for regulating sleep-wake cycles.
Understanding the profound consequences of head injuries on sleep is of immense importance for both medical professionals and those who have experienced such traumas. Unraveling the subtle intricacies of this connection can pave the way for improved diagnostic tools and targeted therapeutic interventions, ultimately offering solace and reprieve to those yearning for a peaceful night's slumber.
Unveiling the Consequences: Exploring the Effects of Traumatic Brain Injuries on Sleep Patterns
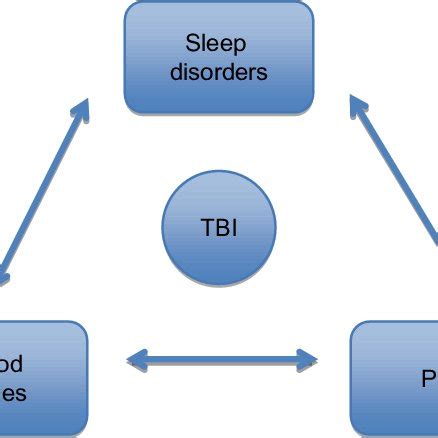
Within the realm of neurological trauma, an inherent connection between the mind and body has been well-established. By delving into the intricate web of repercussions resulting from traumatic brain injuries, a significant aspect requiring comprehensive understanding emerges: the impact on sleep. Beyond the apparent injury lies a complex interplay between cognitive functioning, neurological pathways, and the restorative nature of sleep. Unraveling this connection sheds light on the profound effects these injuries have on an individual's sleep patterns and, ultimately, their overall well-being.
The Sleep-Wake Cycle: A Delicate Balance
Within the realm of head injuries, there lies a significant interplay between sleep and wakefulness. The intricate relationship between these two states of consciousness forms the basis of the sleep-wake cycle, which is crucial for maintaining overall well-being and cognitive function. This section will delve into the delicate balance that exists within this cycle and explore the importance of understanding its dynamics in the context of head injuries.
- 1. The Rhythms of Sleep and Wakefulness
The sleep-wake cycle is characterized by a rhythmic pattern of alternating sleep and wakefulness. During the natural course of a day, the body and mind undergo a synchronized ebb and flow between these states. Sleep is the state of rest and restoration, where the body repairs and regenerates its various systems. In contrast, wakefulness is the active state, where the mind engages with the external environment and carries out various cognitive functions.
- 2. The Role of Circadian Rhythms
A key factor influencing the sleep-wake cycle is the internal biological clock, known as the circadian rhythm. This intrinsic mechanism helps regulate the timing of sleep and wakefulness, ensuring they align with the natural day-night cycle. Disruptions to this delicate balance can negatively impact the quality and duration of both sleep and wakefulness, leading to various health consequences.
- 3. The Impact of Head Injuries on the Sleep-Wake Cycle
Head injuries can profoundly disrupt the delicate balance of the sleep-wake cycle. Traumatic brain injuries, such as concussions, can disrupt the functioning of the internal biological clock, leading to sleep disturbances, excessive sleepiness, and difficulties in maintaining wakefulness. Understanding these effects is crucial in developing appropriate interventions and strategies to mitigate the impact of head injuries on sleep.
- 4. Restoring Balance: Strategies and Interventions
Efforts to restore the delicate balance of the sleep-wake cycle following head injuries are essential for promoting optimal recovery. This section will explore various strategies and interventions aimed at improving sleep quality, managing sleep disturbances, and enhancing wakefulness. By addressing the sleep-wake cycle disruptions, individuals with head injuries can potentially improve their overall well-being and cognitive function.
Consequences of Traumatic Brain Injuries on Sleep Patterns
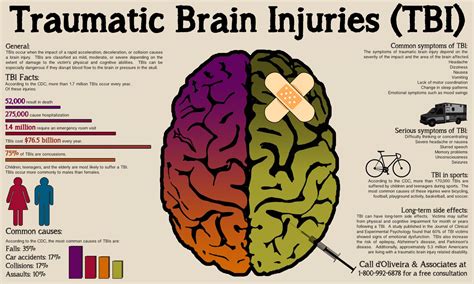
When individuals experience traumatic brain injuries, their sleep patterns can be significantly affected, leading to a range of consequences that impact their overall well-being. The effects of head injuries on sleep can manifest in various ways, causing disturbances in both the quantity and quality of sleep. This article aims to explore the repercussions of such injuries on sleep patterns, highlighting the potential challenges individuals may face in their sleep-wake cycles.
- Insomnia: One common consequence of head injuries is the development of insomnia, where individuals may struggle to fall asleep, stay asleep, or experience non-restorative sleep. This can contribute to feelings of fatigue, irritability, and difficulty concentrating during the day.
- Sleep Fragmentation: Head injuries can disrupt the normal sleep architecture, leading to fragmented sleep patterns. This means that individuals may experience frequent awakenings throughout the night, resulting in a lack of continuous and restful sleep. Sleep fragmentation can further exacerbate daytime sleepiness and cognitive impairments.
- Sleep Disorders: In some cases, head injuries can trigger the onset or exacerbation of existing sleep disorders. For instance, individuals may develop sleep apnea following a traumatic brain injury, leading to interruptions in breathing during sleep that can contribute to further sleep disturbances and daytime symptoms.
- Altered Sleep-Wake Regulation: The brain's ability to regulate sleep and wakefulness can be compromised by head injuries. This can result in abnormal sleep-wake patterns, such as excessive sleepiness during the day or difficulty falling asleep at night. Disruptions in the circadian rhythm may also occur, leading to irregular sleep timing.
- Emotional Disturbances: Head injuries can have a profound impact on emotional well-being, which can, in turn, affect sleep. Individuals may experience increased anxiety, depression, or post-traumatic stress disorder (PTSD) following a traumatic brain injury, leading to difficulties in falling asleep or maintaining a consistent sleep schedule.
Understanding the consequences of head injuries on sleep patterns is crucial for healthcare professionals in providing appropriate care and support for individuals recovering from such injuries. By recognizing and addressing these sleep-related challenges, interventions can be implemented to improve sleep quality and promote overall recovery in individuals with traumatic brain injuries.
How Concussions Disrupt Sleep Architecture
Sleep architecture refers to the organization and structure of sleep stages that occur throughout the night. When a concussion occurs, it can significantly disrupt the normal sleep patterns and cycles, leading to various sleep disturbances and challenges.
One of the primary ways concussions disrupt sleep architecture is through fragmenting sleep. Instead of experiencing a continuous and uninterrupted sleep, individuals with concussions often experience frequent awakenings and difficulty staying asleep. This fragmentation can result in decreased overall sleep quality and an increased likelihood of experiencing daytime sleepiness.
Additionally, concussions can affect the duration and distribution of sleep stages. In normal sleep architecture, there are different stages of sleep, including non-rapid eye movement (NREM) sleep and rapid eye movement (REM) sleep. NREM sleep is further divided into stages 1, 2, and 3, with stage 3 being deep sleep. REM sleep is characterized by vivid dreaming and rapid eye movements. However, concussions can disrupt the normal progression and duration of these sleep stages, leading to an imbalance in sleep architecture.
Furthermore, concussions can also affect the circadian rhythm, which is the internal biological clock that regulates sleep-wake cycles. This disruption can result in difficulties falling asleep or staying asleep at the desired times, leading to sleep deprivation and additional sleep disturbances.
Understanding how concussions disrupt sleep architecture is crucial in developing effective treatment strategies for individuals who have sustained head injuries. By addressing the specific sleep disturbances caused by concussions, healthcare professionals can improve overall sleep quality, promote recovery, and enhance the overall well-being of those affected.
Insomnia and Sleep Disorders: Common Symptoms Following a Traumatic Brain Injury
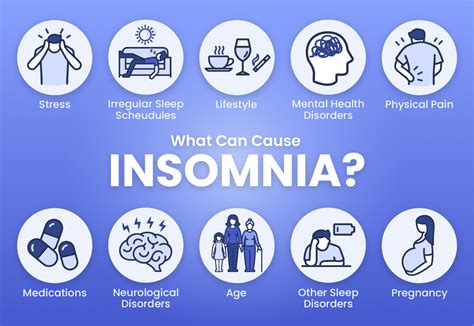
After experiencing a severe blow to the head, individuals often encounter difficulties with their sleep patterns. The consequences of such head injuries can lead to various sleep disorders and insomnia. This section aims to shed light on these common symptoms that arise as a result of a concussion or other traumatic brain injuries.
The aftermath of a head injury can disrupt the delicate balance of the brain's functioning, affecting sleep-wake cycles and giving rise to insomnia. One of the key challenges faced by those with a concussion is falling asleep or staying asleep. The inability to obtain a good night's rest further exacerbates the existing physical and cognitive symptoms, making the recovery process even more challenging.
Individuals who have experienced head injuries may also develop other sleep disorders in addition to insomnia. These sleep disorders include sleep apnea, restless leg syndrome, and narcolepsy. The impact of a traumatic brain injury on the brain's ability to regulate sleep can lead to the development of these disorders, which further compound the difficulties faced by individuals in their daily lives.
| Symptoms | Description |
|---|---|
| Difficulty initiating sleep | Individuals may struggle to fall asleep, spending extended periods lying awake in bed. |
| Difficulty maintaining sleep | Waking up frequently throughout the night, leading to fragmented and inadequate sleep. |
| Early morning awakening | Individuals may consistently wake up earlier than desired and find it challenging to fall back asleep. |
| Daytime sleepiness | Excessive sleepiness during the day, which can interfere with daily activities and overall well-being. |
| Insomnia-related anxiety | The frustration and anxiety associated with persistent insomnia can further disrupt sleep patterns. |
Understanding the prevalence of insomnia and sleep disorders following a concussion is crucial for healthcare professionals and individuals affected by head injuries. By recognizing these common symptoms, appropriate interventions can be implemented to improve sleep quality and enhance overall recovery.
Uncovering the Relationship Between Sleep and Recovery from Brain Trauma
Sleep plays a crucial role in the process of recovering from brain injuries, and understanding this relationship is central to improving patient outcomes. Exploring how sleep impacts the healing and restoration of the brain after trauma can provide valuable insights that can inform effective treatment strategies.
Restorative sleep has been found to have a significant influence on the recovery process following brain injuries, allowing the brain to repair and regenerate damaged tissues. During sleep, the brain engages in various essential processes, such as consolidating memories, clearing toxins, and supporting neural plasticity.
Quality sleep has been shown to promote optimal cognitive functioning, while inadequate sleep can negatively impact memory, attention, and overall cognitive performance. Individuals with brain injuries often experience disruptions in their sleep patterns, such as insomnia or excessive daytime sleepiness. Addressing these sleep disturbances can lead to improved cognitive functioning and overall recovery.
The relationship between sleep and neuroinflammation is an area of ongoing research. Neuroinflammation, a common response to brain injuries, can impede the recovery process. Sleep plays a critical role in regulating inflammation levels, and disturbances in sleep have been linked to increased neuroinflammatory markers. By understanding the impact of sleep on neuroinflammation, researchers can explore potential therapeutic interventions to promote healing and reduce inflammation in the brain.
Developing targeted sleep interventions offers promising opportunities for optimizing the recovery process from brain injuries. Identifying factors that influence sleep quality in individuals with brain trauma, such as pain, anxiety, or medication side effects, can guide the development of tailored interventions. Incorporating techniques such as cognitive-behavioral therapy for insomnia or sleep hygiene practices may help improve sleep quality, leading to enhanced recovery outcomes.
In summary, recognizing the intricate relationship between sleep and recovery from brain injuries reveals the significant role sleep plays in restoring brain function. By delving into this connection, healthcare professionals can develop targeted interventions that promote optimal sleep and ultimately enhance the recovery process for individuals with brain trauma.
Promoting Better Sleep for Patients Recovering from Brain Injury: Effective Strategies and Interventions
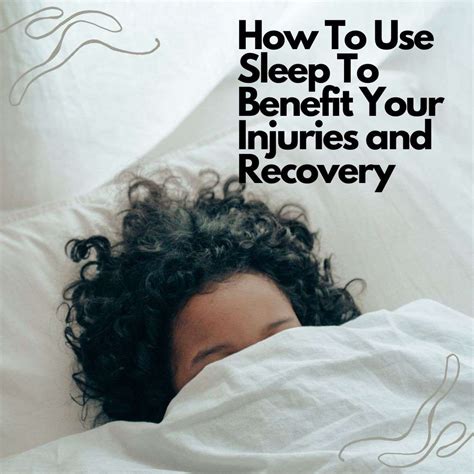
When it comes to aiding in the recovery and overall well-being of individuals who have experienced a brain injury, ensuring proper sleep is crucial. Sleep plays a significant role in the healing process, enabling the brain to rest and restore itself. This section focuses on various strategies and interventions that can be implemented to promote better sleep for concussion patients.
1. Establishing a Consistent Sleep Schedule
- Creating a regular sleep routine can help regulate and maintain the body's natural sleep-wake cycle
- Consistency in bedtime and wake-up times, even on weekends, can improve sleep quality and promote quicker recovery
- Avoiding napping during the day to promote tiredness at night
2. Eliminating Sleep Disruptors
- Reducing exposure to electronic devices (such as smartphones, tablets, and TVs) close to bedtime, as the blue light emitted can interfere with melatonin production
- Minimizing caffeine and alcohol intake, as they can disrupt sleep patterns, especially when consumed close to bedtime
- Creating a calm and comfortable sleep environment, including reducing noise and ensuring a cool, dark room
3. Implementing Relaxation Techniques
- Encouraging deep breathing exercises, progressive muscle relaxation, or guided imagery to promote a relaxed state before bed
- Engaging in activities such as meditation or gentle yoga to calm the mind and reduce anxiety or stress that may interfere with sleep
4. Cognitive Behavioral Therapy for Insomnia (CBT-I)
- Considering CBT-I as an effective non-pharmacological treatment option
- CBT-I focuses on identifying and addressing the underlying causes of insomnia and developing healthy sleep habits and beliefs
- Working with a licensed therapist trained in CBT-I can provide tailored strategies to address specific sleep difficulties
5. Medication and Supplements
- Consulting with a healthcare professional to explore the possibility of short-term medication to address sleep disturbances as part of the recovery process
- Discussing the use of supplements, such as melatonin, valerian root, or magnesium, to support better sleep
- However, it is crucial to consult with a healthcare professional before taking any medication or supplements
By implementing these strategies and interventions, healthcare providers, caregivers, and concussion patients can work together to optimize sleep quality and promote a smoother recovery process. It is essential to remember that every individual's recovery journey is unique, and personalized approaches may be required to address specific sleep challenges effectively.
The Importance of Sleep for Cognitive Function and Emotional Well-being post Brain Injury
Restful sleep plays a crucial role in the recovery process following a traumatic brain injury. This section explores the significant impact of sleep on cognitive function and emotional well-being among individuals who have suffered from brain injuries, focusing particularly on the aftermath of concussions.
Sleep serves as a fundamental pillar for maintaining optimal cognitive abilities, such as attention, memory, problem-solving, and decision-making. After experiencing a brain injury, individuals often encounter disruptions in their sleep patterns, including difficulties falling asleep, staying asleep, or achieving deep sleep stages. These disturbances can have detrimental effects on their cognitive function, leading to cognitive impairments, decreased concentration, memory deficits, and reduced processing speed.
Furthermore, the emotional well-being of individuals who have suffered brain injuries can be significantly impacted by sleep disturbances. Sleep deprivation and poor-quality sleep can contribute to mood dysregulation, increased irritability, anxiety, depression, and an overall decline in emotional resilience. It is essential to recognize the interconnectedness of sleep and emotional regulation, as improving sleep patterns can positively influence emotional well-being and aid in the recovery process.
The disruption of sleep architecture following brain injuries can be attributed to various factors, including changes in neurochemical balance, altered brain connectivity, and physiological effects of the injury itself. Understanding these underlying mechanisms can help healthcare professionals develop effective treatment strategies to address sleep-related issues and promote cognitive recovery and emotional stability.
In conclusion, a comprehensive approach to post-concussion care should prioritize the restoration of healthy sleep patterns. By recognizing the critical role that sleep plays in cognitive function and emotional well-being, healthcare providers can implement interventions specifically designed to improve sleep quality and duration, ultimately assisting individuals in their recovery from brain injuries.
FAQ
What is the connection between head injuries and sleep problems?
Head injuries can disrupt the normal sleep patterns and cause various sleep problems such as insomnia, excessive daytime sleepiness, and sleep fragmentation. These issues can arise due to the impact of the injury on the brain, affecting the hormonal and neurotransmitter balance that regulates sleep-wake cycles.
Are sleep problems a common consequence of head injuries?
Yes, sleep problems are a common consequence of head injuries. Research shows that up to 70% of individuals who have experienced a head injury report sleep disturbances. These disturbances can last for several months or even years, depending on the severity of the injury and the individual's overall health.
What are the long-term effects of head injuries on sleep?
The long-term effects of head injuries on sleep can include persistent insomnia, sleep apnea, excessive daytime sleepiness, and an increased risk of developing sleep disorders such as narcolepsy. These effects can significantly impact an individual's overall quality of life and contribute to other health issues if not properly addressed.
Is there any treatment available for sleep problems caused by head injuries?
Yes, there are treatments available for sleep problems caused by head injuries. Depending on the specific sleep disorder, treatment options may include cognitive behavioral therapy for insomnia, continuous positive airway pressure (CPAP) therapy for sleep apnea, medication for excessive daytime sleepiness, and lifestyle modifications to improve sleep hygiene. It is crucial for individuals to consult with healthcare professionals to determine the most suitable treatment approach.



